Abstract
Introduction: Immune-mediated thrombotic thrombocytopenic purpura (iTTP) is a life-threatening disease with a mortality 10-20% despite emergent therapeutic plasma exchange (TPE). The distinguishing aspect of iTTP from other thrombotic microangiopathies is a severe deficiency of ADAMTS13 (<10% activity) with laboratory evaluation of ADAMTS13 activity often requiring hours to days; thus, it is not useful for determining whether plasma exchange for TTP should be initiated. Guidelines also recommend TPE initiation within 4-8 hours (Scully 2012). There is limited literature regarding utilization of ADAMTS13 testing in the hospital, and we sought to understand ordering patterns in various clinical contexts, which services ordered ADAMTS13 activity, and if TPE initiation was timely.
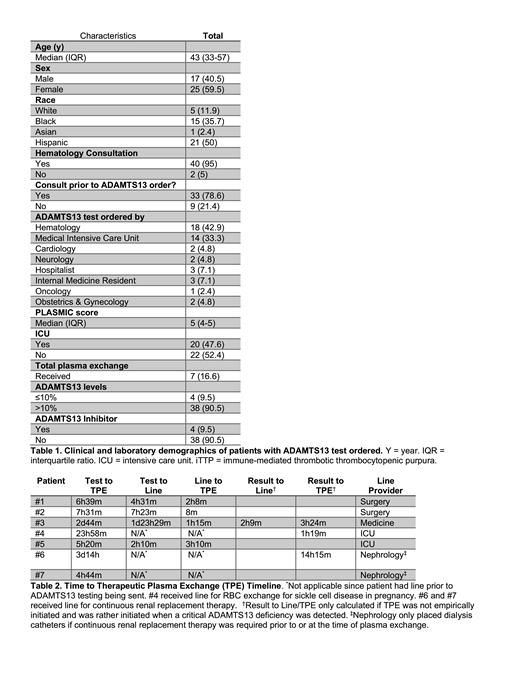
Methods: Parkland Health and Hospital System records were reviewed ADAMTS13 activity tests (n = 361) from January 2019 to March 2021, excluding patients with known iTTP and/or outpatient tests; resulting in a final cohort of 42 patients with inpatient ADAMTS13 activity tests for suspected iTTP. Suspicion for iTTP-time zero for our time to TPE analysis-was determined by the time that the ADAMTS13 order was placed. Hematology consultation time was based on when the order was placed by the provider. The initiation of TPE, as documented by the apheresis team, was the end-time for the time to TPE calculation. Thus, time to TPE was the time elapsed between the electronic ADAMTS13 order being placed and TPE being initiated.
Results: The median patient age was 43 years with 36% Black patients and 50% Hispanic. Hematology service consultation occurred in 95% of cases, although only 79% of hematology consultations occurred before ADAMTS13 activity orders were placed (Table 1). The most common services to order an ADAMTS13 activity prior to hematology consultation were obstetrics and gynecology (2/2, 100%), neurology (1/1, 100%), and medical intensive care (5/14, 36%) with 88% of these tests being placed for patients with a PLASMIC score ≤ 4. None of these patients were diagnosed with iTTP. Using a PLASMIC score ≥6 as a diagnostic test for iTTP, the sensitivity was 50%, specificity 84%, positive predictive value 20%, and negative predictive value was 94%.
A subgroup analysis of patients empirically treated for iTTP (n = 7) demonstrated a wide variation in the time from ADAMTS13 activity orders being placed to initiation of TPE, ranging from 4 hours 44 minutes to 3 days 14 hours (Table 2). Only one patient (without a pre-existing central line) received empiric TPE in under 6 hours (5 hours and 20 minutes). One patient had an ADAMTS13 activity that resulted with a critical ADAMTS13 deficiency and was initiated on TPE; this level was re-analyzed, found to be spurious, and the TPE was ceased immediately. No patients received empiric plasma transfusion.
Discussion: At our county, public hospital, 95% of cases with suspected iTTP involved hematology consultation during their evaluation, but the most common situations where hematology was not involved at all or was involved late were due to non-internal medicine services, identifying areas for focused educational interventions. The PLASMIC score demonstrated insufficient sensitivity (50%) to confidently exclude iTTP, suggesting that it is an inadequate risk stratification tool for our specific patient population. This may be due to differences between our patient population (with a median age of 43 and 12% white patients) and the derivation cohort for the PLASMIC score (with a median age of 51 and 77% white patients; Bendapudi 2017). The finding that only one patient without a pre-existing central line received TPE in ≤6 hours suggests that there is room for quality improvement interventions to hasten time to treatment. This initial study has led to the development of systemic, hospital-wide electronic medical record order set changes combined with educational interventions which will be evaluated prospectively for its impact on iTTP diagnosis and treatment. Broadly, this study re-demonstrates that the evaluation, diagnosis, coordination, and treatment of iTTP is often logistically challenging. Promoting earlier hematology consultation and optimizing EMR interventions is likely to facilitate appropriate ADAMTS13 testing, expedite results, and help coordinate the initiation of TPE in patients with suspected iTTP.
No relevant conflicts of interest to declare.